© 2023 The Trustees of the University of Pennsylvania and IMPaCT Care Inc. All Rights Reserved.
IMPaCT is the leading evidence-based intervention in the U.S. for addressing health inequity and the social determinants of health.
Amid clinical workforce shortages, rising healthcare costs and ongoing concerns about inequity, IMPaCT unlocks the power of the grassroots community health workforce.IMPaCT’s standardized, scalable program transforms the effectiveness of the CHW workforce by reimagining each step, from how to identify the right CHWs, to how to train, develop, manage, and empower them with technology and evidence-based best practices.
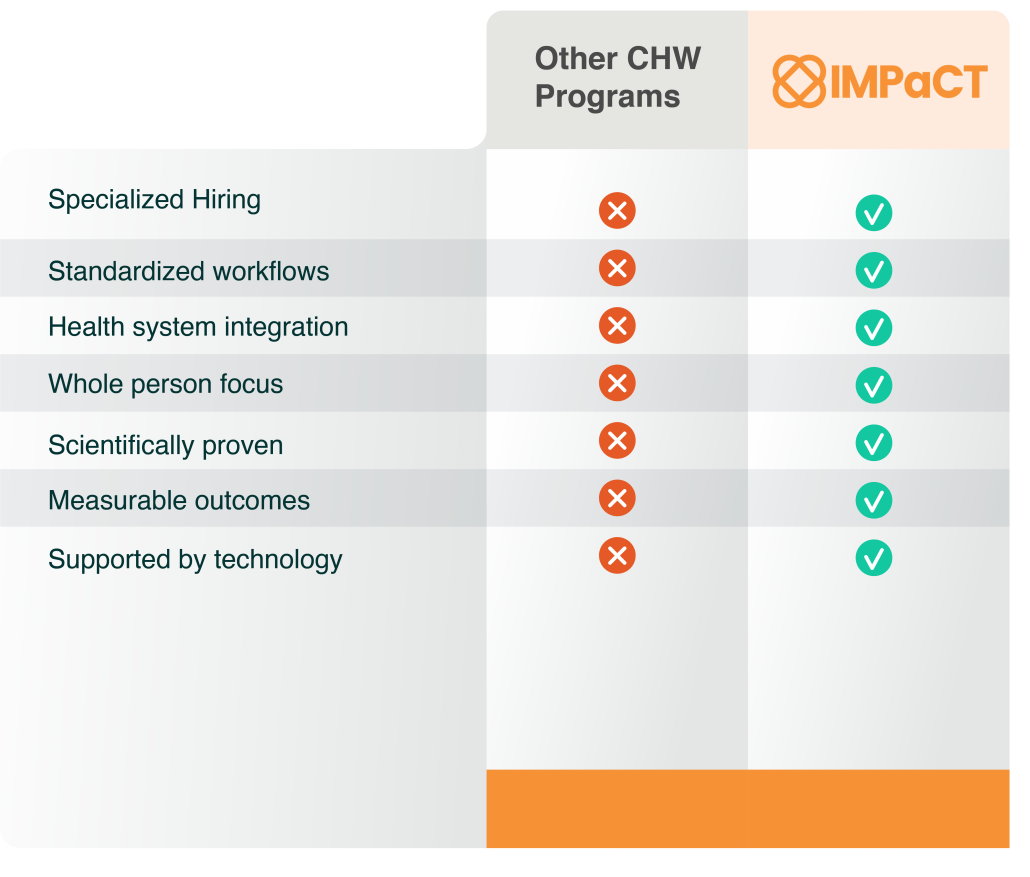
Powered by evidence-based research and cutting-edge technology IMPaCT allows health organizations to staff and manage CHWs at scale.
Expert Consultation and Strategic Planning
Most SDOH programs fail in the planning stage
- We help quickly achieve alignment around defining success and measuring clear benefits.
- We sift through past SDOH successes and failures and provide a gap analysis.
- We guide your risk stratification and population selection.
- We help you develop an internal business case and ROI model.
- Deliver a step-by-step action plan for quick wins.

Network of selected and trained CHWs
Hiring CHWs isn’t like hiring nurses or MAs. Unless you find people with the right heart, turnover rates can be as high as 55-77%.
- We pre-select caring people from local communities screen them for traits like empathy, non-judgement, listening skills and reliability.
- We provide initial training and ongoing professional development for all CHWs –and their supervisors—through the course of their whole career.
- We backfill and train up to 10% turnover at no additional cost.
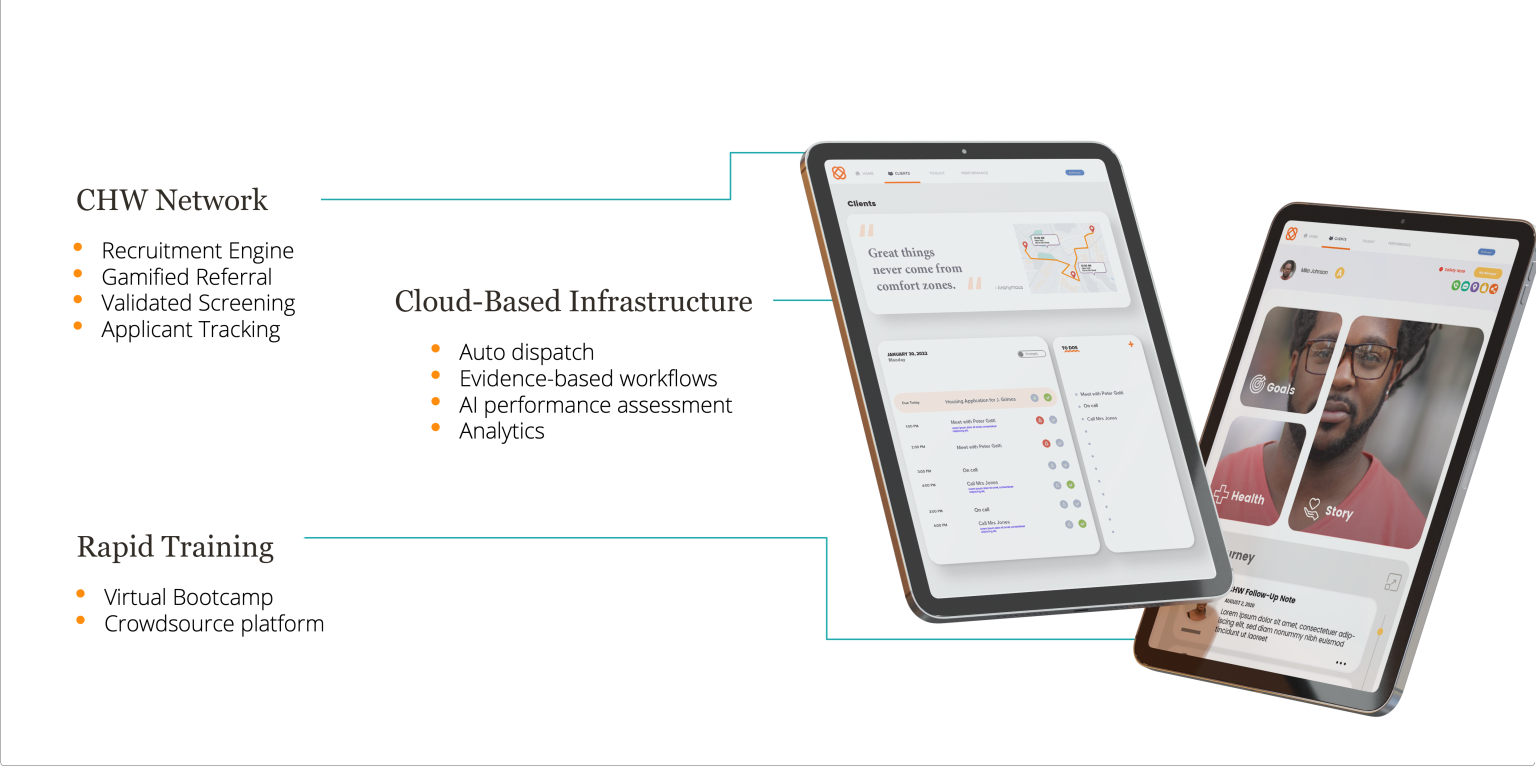
Infrastructure for success and scale
A lot of pieces need to come together to change outcomes for underserved people. CHWs need tools to help them connect with patients, build trust and deliver life-changing results.
- Our application will auto-dispatch patients in need to CHWs. It will automatically load-balance CHW caseloads to avoid burnout or under-performance.
- The application guides CHWs through evidence-based workflows and decision support tools.
- Real-time performance dashboards and analytic insights help to ensure that the workforce is optimized and that you can demonstrate value.

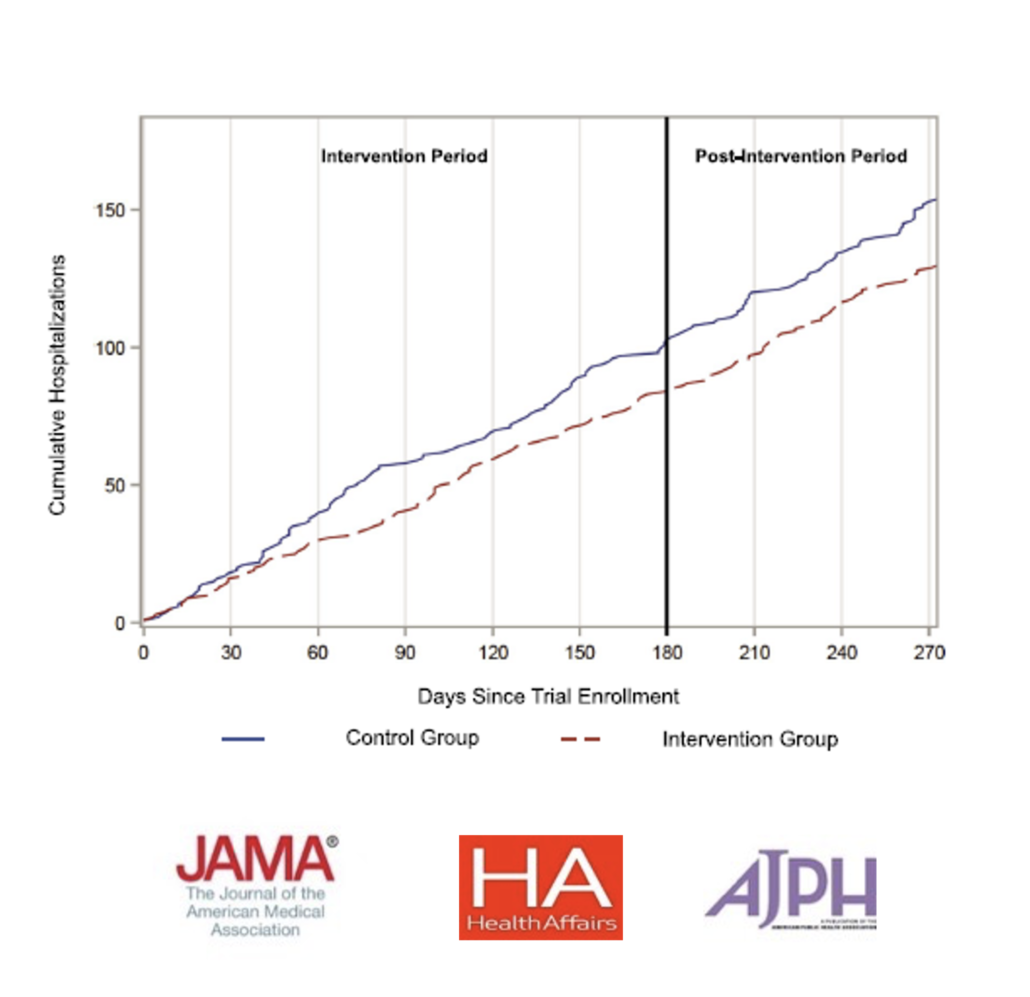
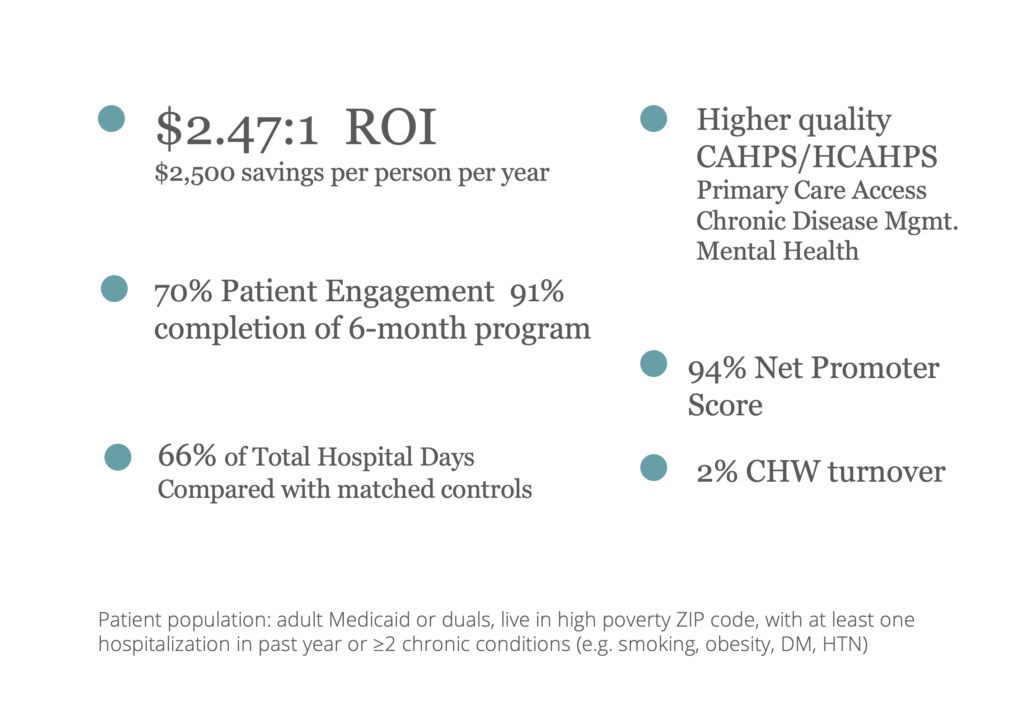
We are RCT-proven on the outcomes everyone cares about.
We’ve achieved outcomes frequently believed to be out of reach: across multiple randomized controlled trials, our team has demonstrated dramatic improvements in cost, health and patient satisfaction – $2,500 saved per patient in year 1, improved mental health, 66% of hospital days compared with matched controls and a 94% net promoter score.
Who you hire makes a critical difference. We find and train empathic people from within local communities who fit a defined profile for success in this role.
Our workflows are evidence-based for achieving strong outcomes. We equip CHWs with an app that connects them to patients in need and guides them to drive change through proven workflows.
You will see improvements in your bottom line: Increase revenue from accurate risk adjustment and quality scores, and reduced hospitalizations and labor costs.

